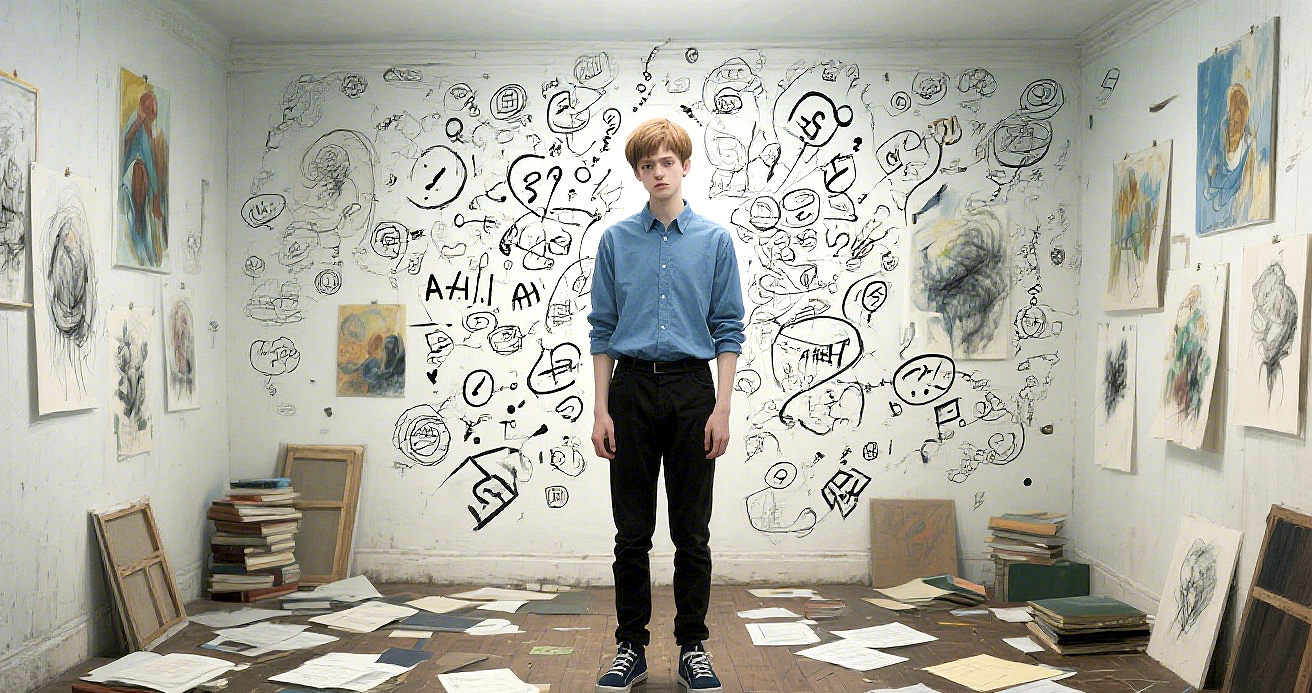
Connecting the Dots: How Clinicians Understand and Assess ADHD
Attention-Deficit/Hyperactivity Disorder (ADHD) is classified in the DSM-5 (Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition) as a neuro-developmental disorder, meaning that it begins in childhood and can continue to affect an individual’s development throughout their life.
ADHD is not simply about being “restless” or “unable to focus.” It affects the brain’s ability to process information, manage emotions, regulate behavior, and organize daily life. Therefore, it is not a sign of laziness, lack of willpower, or insufficient effort. Rather, it is a real, brain-based condition that can be scientifically assessed and supported.
The symptoms of ADHD often persist into adulthood and can significantly impact a person’s relationships, career development, and even personal safety. Due to widespread misunderstandings in society, many individuals do not receive timely or appropriate treatment, preventing them from reaching their full potential.
In adults, ADHD can be especially challenging to diagnose, which makes it harder for them to access effective support. However, once individuals gain a deeper understanding of how their brain works, they often learn to make peace with themselves and find more suitable ways to navigate life’s challenges.
Neuropsychological Explanation:
Attention-Deficit/Hyperactivity Disorder (ADHD) is a neurodevelopmental disorder primarily involving dysregulation within the brain’s executive function network. Research has shown that the prefrontal cortex—particularly the regions responsible for attention control, impulse inhibition, and working memory—exhibits reduced activity or abnormal connectivity, making it difficult for individuals to sustain attention and regulate impulses.
In addition, imbalances in neurotransmitter systems such as dopamine and norepinephrine are believed to play a key role in the manifestation of symptoms. Neuroimaging studies have further confirmed structural and functional differences in these brain regions, revealing the neurobiological foundation of ADHD symptoms.
ASRS-V1.1(Adult ADHD Self-Report Scale Version 1.1)
The Adult ADHD Self-Report Scale Version 1.1 (ASRS-V1.1) is a simple and effective self-screening tool designed to help adults make a preliminary assessment of whether they may have symptoms of Attention-Deficit/Hyperactivity Disorder (ADHD).
Developed collaboratively by the World Health Organization (WHO) and Harvard University, the scale consists of 18 questions that cover two major symptom domains: inattention and hyperactivity/impulsivity. To simplify the screening process, a shorter version with six key questions (known as the “6-item Screener”) is often used to quickly identify individuals who may need further professional evaluation.
Each question asks how often certain symptoms have occurred over the past six months, with response options ranging from “Never” to “Very Often.” Scores are then calculated to produce a total score—the higher the score, the greater the likelihood of ADHD.
Disclaimer: It is important to note that the ASRS-V1.1 is intended only as a preliminary screening tool and cannot replace a professional diagnosis. If your self-assessment indicates a high risk, it is recommended that you consult a qualified physician or mental health professional for a comprehensive evaluation.
Usage rights: Due to copyright and usage restrictions, access to the complete 18-item scale requires official permission from Harvard Medical School. You can visit the Harvard Medical School website to apply for authorization and obtain the full questionnaire for personal use.
Reference:
1. Schweitzer, J.B., Cummins, T.K., Kant, C.A. Attention-deficit/hyperactivity disorder. Med Clin North Am. 2001;85(3):10-11, 757-777. 2. Barkley, R.A. Attention deficit hyperactivity disorder: a handbook for diagnosis and treatment (2nd ed.). 1998. 3. Biederman, J., Faraone, S.V., Spencer, T., Wilens, T., Norman, D., Lapey, K. A, et al. Patterns of psychiatric comorbidity, cognition, and psychosocial functioning in adults with ADHD. Am J Psychiatry. 1993:150:1792-1798. 4. American Psychiatric Association. Diagnostic and statistical manual of mental disorders, (4th ed., text revision). Washington, DC. 2000:85-93.
NICHQ Vanderbilt Assessment Scales
The NICHQ Vanderbilt Assessment Scales is a standardized behavioral evaluation tool developed by the National Institute for Children’s Health Quality (NICHQ).
They are primarily used to assess Attention-Deficit/Hyperactivity Disorder (ADHD) and other related behavioral or emotional issues such as oppositional defiant behavior, conduct problems, anxiety, and depression.
There are two versions of the scales — one completed by parents and the other by teachers — to capture a child’s behavior across different settings. By assessing both the frequency and impact of specific behaviors, the scales help clinicians gather comprehensive and objective background information to:
Conduct preliminary screening and provide clinical support for ADHD diagnosis
Monitor treatment progress and evaluate the effectiveness of medication interventions
Assess how symptoms affect social functioning, such as learning, peer relationships, and self-regulation
The scales include multiple domains that measure attention, impulse control, activity level, academic performance, and peer interactions. Results serve as supportive data for professionals to make an informed, comprehensive evaluation.
It’s important to note that the Vanderbilt ADHD Assessment Scales are intended for screening and reference purposes only. They do not replace a professional medical evaluation or serve as a formal diagnosis. The results reflect the rater’s observations of the child’s current behaviors and should not be interpreted as definitive evidence of a disorder.
If you have concerns about the results or suspect that your child may have attention, emotional, or behavioral difficulties, please consult a qualified child psychologist or psychiatrist for a thorough professional assessment.
Reference: American Academy of Pediatrics, & National Initiative for Children's Healthcare Quality. (2002). NICHQ Vanderbilt Assessment Scales. The National Institute for Children's Health Quality.
DSM 5 - Attention-Deficit/Hyperactivity Disorder
Disorder Class: Neurodevelopment Disorders
A. A persistent pattern of inattention and/or hyperactivity-impulsivity that interferes with functioning or development, as characterized by (1) and/or (2):
Inattention: Six (or more) of the following symptoms have persisted for at least 6 months to a degree that is inconsistent with developmental level and that negatively impacts directly on social and academic/occupational activities:
(NOTE: The symptoms are not solely a manifestation of oppositional behavior, defiance, hostility, or failure to understand tasks or instructions. For older adolescents and adults (age 17 or older), at least five symptoms are required.)
a. Often fails to give close attention to details or makes careless mistakes in schoolwork, at work, or during other activities (e.g., overlooks or misses details, work is inaccurate).
b. Often has difficulty sustaining attention in tasks or play activities (e.g., has difficulty remaining focused during lectures, conversations, or lengthy reading).
c. Often does not seem to listen when spoken to directly (e.g., mind seems elsewhere, even in the absence of any obvious distraction).
d. Often does not follow through on instructions and fails to finish schoolwork, chores, or duties in the workplace (e.g., starts tasks but quickly loses focus and is easily sidetracked).
e. Often has difficulty organizing tasks and activities (e.g., difficulty managing sequential tasks; difficulty keeping materials and belongings in order; messy, disorganized work; has poor time management; fails to meet deadlines).
f. Often avoids, dislikes, or is reluctant to engage in tasks that require sustained mental effort (e.g., schoolwork or homework; for older adolescents and adults, preparing reports, completing forms, reviewing lengthy papers).
g. Often loses things necessary for tasks or activities (c.g., school materials, pencils, books, tools, wallets, keys, paperwork, eyeglasses, mobile telephones).
h. Is often easily distracted by extraneous stimuli (for older adolescents and adults, may include unrelated thoughts).
i. Is often forgetful in daily activities (eg, doing chores, running errands; for older adolescents and adults, returning calls, paying bills, keeping appointments).
2. Hyperactivity and impulsivity: Six (or more) of the following symptoms have persisted for at least 6 months to a degree that is inconsistent with developmental level and that negatively impacts directly on social and academic/occupational activities:
(NOTE: The symptoms are not solely a manifestation of oppositional behaviour, defiance, hostility, or a failure to understand tasks or instructions. For older adolescents and adults (age 17 or older), at least five symptoms are required.)
a. Often fidgets with or taps hands or feet or squirms in seat.
b. Often leaves scat in situations when remaining seated is expected (c.g., leaves his or her place in the classroom, in the office or other workplace, or in other situations that require remaining in place).
c. Often runs about or climbs in situations where it is inappropriate. (Note: In adolescents or adults, may be limited to feeling restless).
d. Often unable to play or take part in leisure activities quietly.
e. Is often "on the go" acting as if "driven by a motor" (c.g., is unable to be or uncomfortable being still for extended time, as in restaurants, meetings; may be experienced by others as being restless or difficult to keep up with).
f. Often talks excessively.
g. Often blurts out an answer before a question has been completed (c.g., completes people's sentences; cannot wait for turn in conversation).
h. Often has trouble waiting his/her tum (c.g., while waiting in line).
i. Often interrupts or intrudes on others (c.g., butts into conversations, games, or activities; may start using other people's things without asking or receiving permission; for adolescents and adults, may intrude into or take over what others are doing).
B. Several inattentive or hyperactive-impulsive symptoms were present before age 12 years.
C. Several inattentive or hyperactive-impulsive symptoms are present in two or more settings, (c.g., at home, school or work; with friends or relatives; in other activities).
D. There is clear evidence that the symptoms interfere with, or reduce the quality of, social, school, or work functioning.
E. The symptoms do not occur exclusively during the course of schizophrenia or another psychotic disorder and are not better explained by another mental disorder (c.g., mood disorder, anxiety disorder, dissociative disorder, personality disorder, substance intoxication or withdrawal).
Specify whether:
Combined presentation: If enough symptoms of both criteria inattention and hyperactivity-impulsivity were present for the past 6 months Predominantly inattentive presentation: If enough symptoms of inattention, but not hyperactivity-impulsivity, were present for the past 6 months Predominantly hyperactive-impulsive presentation:
If enough symptoms of hyperactivity-impulsivity but not inattention were present for the past 6 months.
Specify if:
In partial remission: When full criteria were previously met, fewer than the full criteria have been met for the past 6 months, and the symptoms still results in impairment in social, academic, or occupational functioning.
Specify current severity:
Mild: Few, if any, symptoms in excess of those required to make the diagnosis are present, and symptoms result in no more than minor impairments in social or occupational functioning. Moderate: Symptoms or functional impairment between "mild" and "severe" are present. Severe: Many symptoms in excess of those required to make the diagnosis, or several symptoms that are particularly severe, are present, or the symptoms result in marked impairment in social or occupational functioning.
Reference: Center for Behavioural Health Statistics and Quality. (2016). 2014 National Survey on Drug Use and Health: DSM-5 Changes: Implications for Child Serious Emotional Disturbance (unpublished internal documentation). Substance Abuse and Mental Health Services Administration, Rockville, MD.
If you’re looking for mental health support for ADHD symptoms, feel free to reach out. If you need a formal assessment, I’d be happy to help connect you with a psychologist in Edmonton.
@
If you’re looking for mental health support for ADHD symptoms, feel free to reach out. If you need a formal assessment, I’d be happy to help connect you with a psychologist in Edmonton. @
ADHD Assessment Process
Disclaimer:
The following process may vary depending on clinical practice standards and guidelines. The steps outlined below are intended as a general overview and should not be interpreted as a description of specific or standardized clinical procedures.**
Initial Screening
Our process begins with an initial interview to explore whether ADHD may be contributing to challenges in emotional regulation, focus, relationships, or work/school performance. Using DSM-5 criteria, I will review your presenting concerns, identify possible ADHD symptoms, and determine whether a comprehensive evaluation is the next step.
Comprehensive Evaluation
If further assessment is appropriate, we move into a more detailed evaluation that includes in-depth interviews and self-report measures. This stage is designed to build a full picture of your experience — not just the symptoms, but the story behind them.
For children or teens, I meet with parents or caregivers to gain additional perspectives; for adults, I may include partners or family members who know you well. Together, we’ll explore:
What specific symptoms are showing up and when they began
The settings where these challenges occur (home, school, work, relationships)
How long symptoms last and what may trigger or ease them
How much these symptoms interfere with your daily life and goals
Bio-Psycho-Social Understanding
We’ll complete a holistic assessment that looks beyond behaviour to understand the full context of your life. Areas we may discuss include:
Developmental, medical, and family history
Emotional wellbeing and any co-occurring concerns (e.g., anxiety, depression, learning difficulties)
Strengths, talents, and coping skills
Academic or work experiences
Relationships, family dynamics, and social connections
Temperament, personality, and current functioning
For children, this may include a play-based or behavioural observation
Rating Scales and Collaborative Input
I use standardized ADHD behaviour and self-report rating scales to gather measurable insights. When helpful, I may also request input from others who interact closely with you — such as family members, teachers, or colleagues — to better understand how symptoms show up in daily life.
Additional Assessments (as needed)
Depending on your presentation, I may refer you for complementary evaluations to ensure a thorough understanding. These may include:
Medical or neurological screening
Psychiatric consultation for co-occurring disorders or medication evaluation
Psychological testing for learning differences
Vision, hearing, or speech-language screening
Review & Collaborative Planning
Once all information is collected, we’ll meet to review results, including rating scales, relevant records, and observations. I will share a clear summary of findings and discuss whether ADHD or other factors best explain your challenges. Together, we will create a tailored treatment plan focused on your strengths, goals, and long-term wellbeing.
Differential Consideration
Because ADHD can overlap with or resemble other conditions, I take special care to screen for related or co-occurring concerns such as:
Anxiety or mood disorders
Trauma-related symptoms
Learning disabilities
Autism spectrum traits
Personality or impulse-control disorders
Substance use patterns
Medical or neurological factors